Rajni Sharma – A 50-year-old woman from Jammu had been suffering from auto-immune liver disease for the past 2 years. She got a new lease of life when she came to Dr Vivek Vij – the best liver transplant doctor in India.
Curious to get deep insights into Rajni Sharma’s journey with Dr Vivek Vij? We have got you covered. Read this blog to find out more.
A 50-year-old woman from Jammu had been suffering from auto-immune liver disease for the last 2 years and desperately required liver transplant surgery as the complications were rising day by day.
She was frail, had water retention in her stomach, and her appetite had diminished. Due to this, she also started feeling very weak and her immunity had taken a serious toll. She also had Hepatic Encephalopathy, in which the liver problems start affecting the mind. Due to this, she felt more sleepy, agitated, and suffered sleep reversal among other things.
When she consulted a doctor in Jammu, that doctor suggested she visit Dr Vivek Vij – the best liver transplant doctor in India. After that, the patient’s family also read about Dr Vivek Vij on the internet and was very impressed by his history and experience. They learned that Dr Vivek Vij has done many successful liver transplant surgeries and given new life to many liver patients.
So, the family and patient decided to get a consultation from Dr Vivej Vij. When patient Rajni came to Dr Vivek Vij, they got very good treatment from the doctors. The team of doctors analysed the patient’s situation and did a detailed session with the family and the patient, and they agreed upon the liver transplantation. Mrs. Rajni’s daughter became her donor for the transplant.
Her liver transplant was performed on 22 October, after her admission, and she was discharged within three weeks. Now Mrs Rajni is living a healthy life, and her problem is also treated.
After watching this video, you might be curious to know more about Auto-immune liver disease. If yes, let’s understand more about Autoimmune Hepatitis causes, symptoms, treatments and many more.
When the body’s immune system attacks the liver and causes inflammation, autoimmune liver hepatitis develops. It may result in liver cell destruction and, ultimately, liver failure. Fatigue, stomach pain, jaundice (yellowing of the skin and eyes), and dark urine fall under autoimmune hepatitis symptoms.
The exact autoimmune hepatitis causes are unknown, but it is supposed to be a combination of genetic and environmental factors. It is typically treated with corticosteroids and immunosuppressive medicines to lessen inflammation and slow disease progression.
Some of the symptoms listed below are possible in people with autoimmune hepatitis:
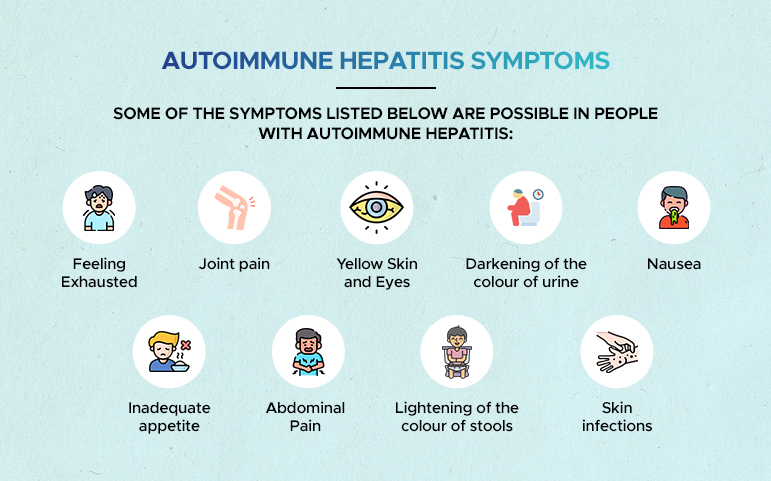
When symptoms of autoimmune liver disease are present, they can vary from mild to extreme.
Some victims of autoimmune liver hepatitis show no signs of the disease. In these situations, doctors may detect liver issues during routine blood testing, which results in the identification of autoimmune liver disease. Those who are diagnosed without symptoms may subsequently start to experience them.
Some people living with autoimmune hepatitis don’t exhibit symptoms until consequences from cirrhosis appear. These signs include
There are two basic types of autoimmune hepatitis stages, according to doctors.
The exact autoimmune hepatitis causes are unknown, but it is considered to be a combination of genetic and environmental elements. Some possible causes include the following:
It is worth mentioning that autoimmune liver disease can appear in children and adults, and it is more familiar in women than in men. It is also possible to have autoimmune hepatitis and other autoimmune disorders such as Lupus, Rheumatoid arthritis and others.
The diagnosis of autoimmune liver hepatitis typically involves a combination of tests and evaluations, which may have:
Chronic autoimmune hepatitis can be a serious ailment. Although there is no treatment, it can be controlled and put into remission. Remission indicates that the disease is not active or showing symptoms. Treatment for AIH frequently combines several methods.
These medications can diminish or even stop your immune system’s attack on your body. The immunosuppressants 6-mercaptopurine and azathioprine are frequently used to treat AIH.
When taken in large amounts, corticosteroid drugs can diminish immune system activity and lessen body inflammation. They can be taken orally, topically, intravenously, or breathed. Prednisone taken orally is the corticosteroid most frequently used for AIH. Prednisone is frequently recommended for a minimum of 18 to 24 months in order to minimise liver inflammation.
A liver transplant is required in severe cases of AIH. Your complete liver will be removed during this treatment, and a donor liver will be used instead (the donor may be alive or deceased). Nevertheless, the illness can occasionally come back even after a successful transplant.
Now, let’s go through some details of hepatic liver encephalopathy.
Hepatic Encephalopathy (HE) is an ailment that occurs when the liver is not able to release toxins from the blood effectively. These toxins can then build up in the brain, directing to changes in behaviour, cognitive function, and consciousness.
Signs of Hepatic Encephalopathy can vary from mild disorder and sleep disorders to severe shifts in mental function, such as comma. The condition is typically caused by liver cirrhosis (scarring of the liver) but can also transpire due to other liver disorders, infections, or metabolic ailments.
Hepatic Encephalopathy treatment options may include medicines, dietary shifts, and the removal of toxins through blood filtration. In extreme cases, a liver transplant may be required.
Hepatic Encephalopathy can be of three different types:
The exact cause of Hepatic Encephalopathy is unspecified. However, an accumulation of toxins in the bloodstream typically causes it to develop. It happens when your liver is unable to break down toxins effectively.
Hepatic Encephalopathy may be activated by the following:
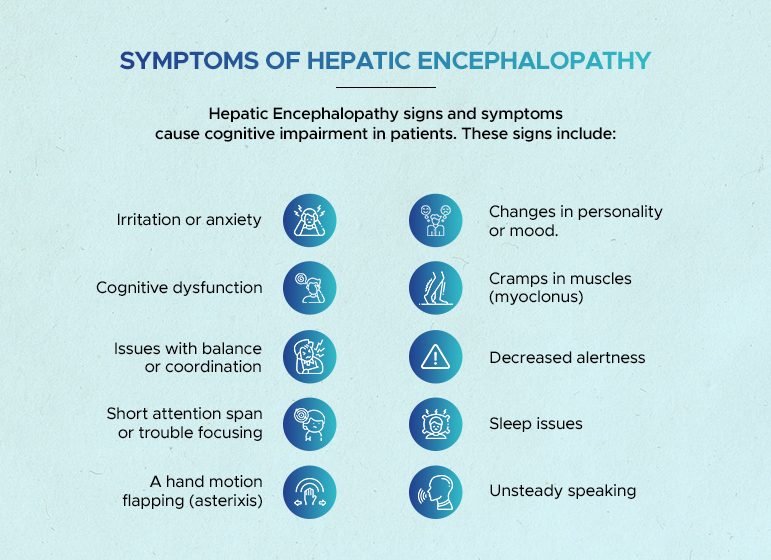
Hepatic Encephalopathy signs and symptoms cause cognitive impairment in patients. These signs include:
A physical examination, a discussion of the patient’s symptoms, and a review of their medical history serve as the first steps in the diagnostic process for Hepatic Encephalopathy. These techniques might be sufficient to diagnose Hepatic Encephalopathy in some situations.
In other situations, a physician may request one or more tests to determine Hepatic Encephalopathy’s symptoms. These tests, as examples, include:
Treatment for Hepatic Encephalopathy relies on the type and severity of the infection but generally includes a variety of medical and lifestyle interventions. Some standard treatment options include:
It’s worth mentioning that some medicines used to treat Hepatic Encephalopathy can have side effects and may not be appropriate for everyone. Hence, working closely with a healthcare provider to find the most suitable treatment plan is essential.
Also, continuous monitoring and follow-up are crucial for those with liver Encephalopathy to guarantee the condition doesn’t deteriorate and to adjust treatment accordingly.
So if you are looking for the best treatment for any of your liver conditions, get the best consultation from Dr Vivek Vij. He is the top Liver Transplant Surgeon in india who has done thousands of successful liver transplantations. AILBS India has Liver Transplant Success Rate in India and the top liver transplant hospital in India dedicated to giving you the best ever treatment for all your liver conditions.